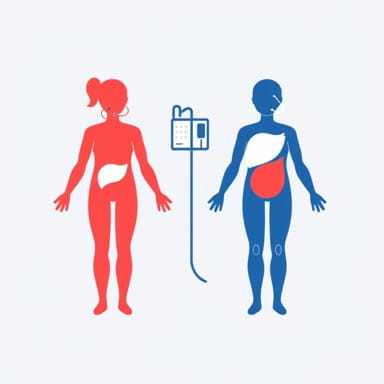
When the kidneys fail to work properly, dialysis becomes a life-saving option that helps remove waste products and excess fluids from the blood. Two of the most commonly used types of dialysis are hemodialysis and peritoneal dialysis. While both serve the same ultimate purpose, they differ in method, lifestyle impact, and overall approach to treatment. Understanding the differences between hemo vs peritoneal dialysis is essential for patients and families in order to make informed decisions about care. Each method has unique benefits, potential complications, and considerations that can affect daily life and long-term health outcomes.
What is Hemodialysis?
Hemodialysis, often shortened to hemo, is a process where a machine outside the body performs the work of filtering blood. This procedure requires a vascular access point, usually created through a fistula, graft, or catheter. The patient’s blood flows into a dialysis machine, where a special filter called a dialyzer cleans the blood before it is returned to the body. Hemodialysis usually takes place in a dialysis center, although some patients may perform it at home with the right equipment and training.
How Hemodialysis Works
During hemodialysis, two needles are placed into the vascular access site. One needle carries blood to the dialyzer, while the other returns the cleaned blood back into the body. The dialyzer uses a semi-permeable membrane and a special dialysis fluid to remove waste, extra salts, and water. A typical hemo session lasts about three to five hours and is usually done three times per week.
Advantages of Hemodialysis
- Effective at removing waste products quickly.
- Treatment is supervised by medical staff in a clinical setting.
- Patients have regular check-ins with healthcare providers.
- Does not require daily treatment sessions at home.
Disadvantages of Hemodialysis
- Requires regular visits to a dialysis center unless performed at home.
- Each session can be time-consuming and tiring.
- Dietary and fluid restrictions are often strict.
- Needle insertion may be uncomfortable for some patients.
What is Peritoneal Dialysis?
Peritoneal dialysis, also known as PD, uses the lining of the abdominal cavity, called the peritoneum, as a natural filter. Instead of using a machine to filter blood outside the body, a cleansing fluid is introduced into the abdominal cavity through a catheter. Waste and excess fluid move from the blood into the dialysis fluid, which is then drained and replaced with fresh solution. This process can be done at home, and sometimes even while sleeping, giving patients greater flexibility.
How Peritoneal Dialysis Works
A soft tube, known as a catheter, is surgically placed into the abdomen. Dialysis fluid is poured into the abdominal cavity and left there for several hours while waste products pass from the blood into the fluid. Afterward, the fluid is drained and replaced. This cycle is called an exchange. Patients can perform exchanges manually several times a day (Continuous Ambulatory Peritoneal Dialysis, or CAPD) or use a machine at night (Automated Peritoneal Dialysis, or APD).
Advantages of Peritoneal Dialysis
- Can be performed at home, reducing the need for frequent hospital visits.
- Provides more flexibility and independence in daily life.
- No needles are required for each session.
- Dietary restrictions may be less strict compared to hemo.
Disadvantages of Peritoneal Dialysis
- Requires daily treatment and responsibility for cleanliness.
- Risk of infection at the catheter site or inside the abdomen (peritonitis).
- May not be as effective for patients with larger body sizes or certain medical conditions.
- Storage space is needed for dialysis supplies at home.
Comparing Hemo vs Peritoneal Dialysis
When discussing hemo vs peritoneal dialysis, it is important to note that both methods aim to extend life and improve quality of health for patients with kidney failure. However, the choice often depends on lifestyle, personal preference, medical condition, and access to resources.
Lifestyle Considerations
Hemodialysis requires scheduling around fixed clinic visits, which can limit flexibility but provides professional monitoring. Peritoneal dialysis, on the other hand, can be done at home, allowing more freedom but also demanding personal responsibility. Patients who value independence may lean toward PD, while those who prefer structured medical oversight may choose hemo.
Medical Effectiveness
Hemodialysis is usually more efficient at rapidly clearing waste products, which is beneficial in acute situations. Peritoneal dialysis, however, works more gradually and continuously, which can be gentler on the body and heart. Some patients may start with PD and later transition to hemo as their condition changes.
Potential Complications
In hemodialysis, risks include low blood pressure during sessions, muscle cramps, and vascular access issues. In peritoneal dialysis, infection remains the main concern. Both types of dialysis can have long-term effects on the body, such as weakening of bones and anemia, requiring additional treatment and monitoring.
Choosing the Right Dialysis Method
Deciding between hemo vs peritoneal dialysis involves weighing personal lifestyle, health condition, and comfort level with self-care. Doctors often consider age, medical history, and home environment before recommending a treatment plan. Some patients may even try both methods before deciding which fits best. Ultimately, dialysis is not one-size-fits-all, and treatment should be customized to meet the patient’s unique needs.
Both hemodialysis and peritoneal dialysis are effective ways to manage kidney failure. Hemodialysis provides structured care and strong waste removal but comes with time commitments and lifestyle restrictions. Peritoneal dialysis offers independence and flexibility, yet it requires discipline and carries infection risks. Understanding hemo vs peritoneal dialysis in detail allows patients and families to make informed choices that balance health, convenience, and quality of life. With proper support and medical guidance, both methods can help individuals live longer, healthier, and more fulfilling lives despite kidney disease.