Hard calcium deposits underneath the skin can be concerning for many people, especially when they appear suddenly or grow over time. These deposits often feel like firm lumps beneath the surface and may vary in size and number. While they are not always painful, they can cause discomfort, skin irritation, or even limit movement if they develop near joints. Understanding why calcium builds up in soft tissues, what conditions are associated with these deposits, and how they are diagnosed and managed can help individuals make informed decisions about their health and treatment options.
What Are Hard Calcium Deposits Underneath the Skin?
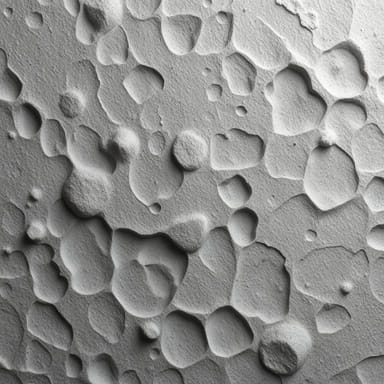
Calcium deposits under the skin, also calledcalcinosis cutis, occur when calcium salts accumulate in the skin and underlying tissues. Unlike the normal role of calcium in bones and teeth, where it provides strength and structure, abnormal deposits in soft tissues indicate an imbalance or underlying medical condition. These deposits may appear as small nodules, plaques, or larger lumps that are visible through the skin or palpable when touched.
Types of Calcinosis Cutis
Medical experts classify calcium deposits into different categories based on their underlying causes. Each type has unique characteristics and associations with certain health conditions.
- Dystrophic calcinosisOccurs in areas of damaged or inflamed tissue, often associated with autoimmune diseases such as lupus or dermatomyositis.
- Metastatic calcinosisCaused by high levels of calcium or phosphate in the blood, often related to kidney disease, hormonal imbalances, or certain metabolic disorders.
- Iatrogenic calcinosisResults from medical treatments, such as repeated calcium-containing injections or intravenous therapy.
- Idiopathic calcinosisAppears without an identifiable underlying cause, more common in otherwise healthy individuals.
Causes of Calcium Deposits Beneath the Skin
Several factors can contribute to the development of hard calcium deposits. The cause often determines the severity and treatment approach. Common causes include
- Chronic inflammation or tissue injury
- Autoimmune conditions such as scleroderma or lupus
- Kidney disease that affects calcium and phosphate balance
- Hyperparathyroidism, which leads to excess calcium in the blood
- Genetic conditions that disrupt calcium metabolism
- Infections or trauma to the skin
Symptoms of Hard Calcium Deposits Underneath the Skin
While some calcium deposits cause little to no symptoms, others can lead to noticeable issues depending on their size and location. Common symptoms include
- Firm or hard nodules beneath the skin
- Redness, swelling, or tenderness around the deposit
- Ulceration or skin breakdown if the deposits erode the surface
- Pain during movement if deposits are near joints or muscles
- Restricted mobility in severe cases
Who Is Most at Risk?
Not everyone develops calcium deposits under the skin, but certain groups are at higher risk. These include people with autoimmune disorders, chronic kidney disease, or imbalances in calcium and phosphate levels. Children and young adults may experience idiopathic deposits, while older adults are more likely to develop deposits due to age-related conditions and long-term illnesses.
Diagnosis of Calcium Deposits
Diagnosing calcium deposits requires a combination of physical examination and medical imaging. Doctors may use X-rays, ultrasound, or CT scans to confirm the presence and extent of deposits. Blood tests are often performed to measure calcium and phosphate levels and to check for autoimmune markers or kidney function. In some cases, a skin biopsy may be needed to confirm the diagnosis and rule out other conditions.
Complications of Untreated Deposits
Although not all deposits require treatment, ignoring them can sometimes lead to complications. These may include
- Chronic skin irritation or ulceration
- Secondary bacterial infections
- Joint stiffness or mobility issues
- Disfigurement or cosmetic concerns
- Persistent pain and inflammation
Treatment Options for Hard Calcium Deposits
Treatment depends on the underlying cause, the severity of the deposits, and the symptoms experienced by the patient. Some deposits may remain stable and require only observation, while others need medical or surgical intervention.
Medications
Doctors may prescribe medications to manage symptoms or slow the growth of deposits. Options include
- Anti-inflammatory drugs to reduce pain and swelling
- Medications that regulate calcium and phosphate levels
- Drugs used in autoimmune conditions to suppress abnormal immune activity
Non-Surgical Therapies
In some cases, treatments such as laser therapy, shockwave therapy, or topical ointments may help reduce the size of deposits or ease discomfort. These approaches are usually recommended when deposits are small and not deeply embedded in tissue.
Surgical Removal
When calcium deposits cause significant pain, interfere with movement, or repeatedly lead to skin breakdown, surgical removal may be necessary. Dermatologists or surgeons can excise the nodules, although recurrence is possible if the underlying cause is not addressed.
Lifestyle and Self-Care Strategies
In addition to medical treatment, lifestyle changes can play a role in preventing or managing calcium deposits. Some helpful strategies include
- Maintaining a balanced diet with appropriate calcium and phosphate intake
- Managing chronic conditions like kidney disease or autoimmune disorders
- Protecting the skin from repeated trauma or injury
- Staying hydrated to support kidney function
- Following up regularly with healthcare providers for monitoring
When to Seek Medical Help
While some calcium deposits may not cause serious issues, medical attention is necessary if the deposits grow rapidly, become painful, or cause skin ulceration. Early evaluation helps prevent complications and ensures that the underlying cause is identified and treated properly.
Outlook and Long-Term Management
The outlook for individuals with calcium deposits varies widely depending on the cause. People with deposits related to autoimmune disease may experience recurring issues, while those with isolated deposits may have complete resolution after treatment. Long-term management often involves regular monitoring and controlling underlying health conditions to minimize recurrence.
Hard calcium deposits underneath the skin are a complex condition that can range from minor cosmetic concerns to painful, movement-limiting problems. They are influenced by multiple factors, including autoimmune diseases, kidney function, and metabolic imbalances. Early diagnosis and proper treatment can significantly improve quality of life, while lifestyle strategies can help reduce the risk of recurrence. Recognizing the signs, understanding the causes, and seeking timely medical care are essential steps for anyone dealing with this condition.
By learning more about calcinosis cutis and its management, individuals can take control of their health and address not only the deposits themselves but also the underlying conditions that may contribute to their development.